Attention
Enrollments for 837 EDI, 835 ERA, and EFT are now available! Currently, 835 ERA enrollments for TRICARE Overseas, 270 batch/real-time, 276 batch/real-time, 820, and 834 are still under construction.
Updates coming soon!
Attention
A valid WPS EDI Trading Partner ID is required to ensure timely processing of your Electronic Remittance Advice (ERA).
Save time and money by enrolling in paperless electronic transactions. Trading partners also use this link to add new lines of business and transactions when enrolling a new provider.
If you need to deactivate or reactivate an existing enrollment for an electronic transaction, please call the correct EDI area depending on your benefit/insurance.
Learn more about the EDI process—If you are unfamiliar with the EDI process, WPS strongly encourages you to learn more by visiting our Getting Started page.
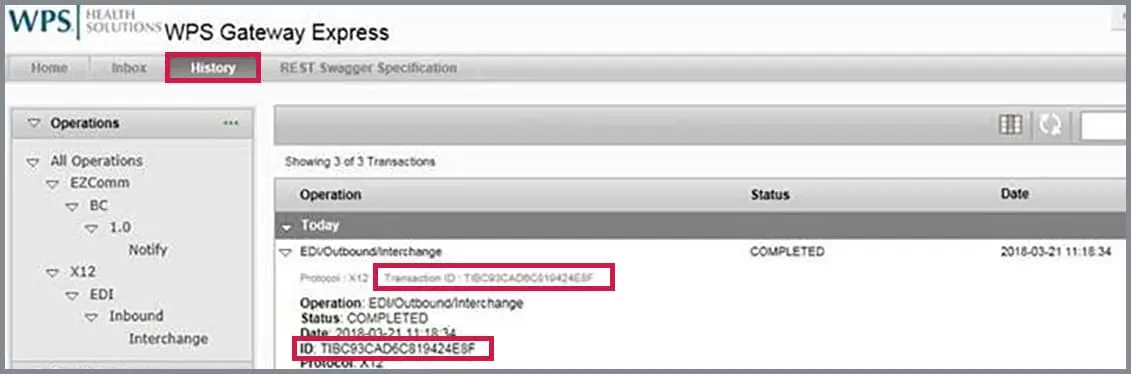
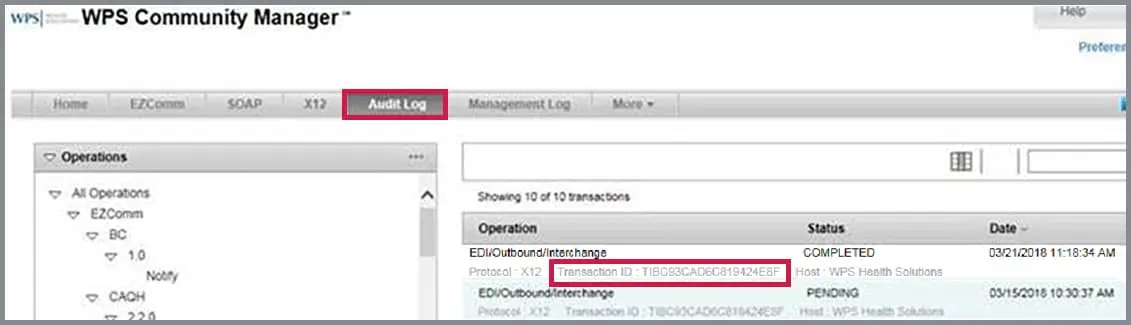
Instructions to find the Transaction ID are available on this link.
You can locate the Transaction ID in the History view in WPS Gateway Express
Or, in the Audit Log view view in the WPS Community Manager
Please read more below for information on the available WPS portals for each benefit or insurance WPS offers.
TRICARE East Region Online Claim Submissions
No LIVE claims submissions to WPS from current TRICARE East Region providers are allowed until Jan. 1, 2018.
Qualified TRICARE East Region providers can enter claims into the portal for transmission to WPS and view remittance advices.
To submit TRICARE East Region claims on the Humana Military secured provider portal, you must be enrolled in HumanaMilitary.com (go to Provider > Resources > Self-Service).
If you are already enrolled, initiate submitting claims for TRICARE East Region.
WPS Government Health Administrators Online Portal Claim Submissions
Qualified Medicare providers can enter individual Part B claims into the portal for transmission to WPS and view remittance advices for individual Part B claims.
To submit Part B claims on the WPS Government Health Administrators portal:
View instructions to initiate submitting claims in WPS Government Health Administrators Portal.
TRICARE4U.com Online Claim Submissions
Qualified TRICARE For Life providers can enter claims into the portal for transmission to WPS and view remittance advices by patient number or check number.
To submit TRICARE For Life claims on the TRICARE4U.com provider portal:
If you are already enrolled, initiate submitting claims for TRICARE For Life.
TRICARE-Overseas.com Online Claim Submissions
Qualified TRICARE Overseas providers can enter claims into the portal for transmission to WPS and view remittance advices by patient number or check number.
To submit TRICARE Overseas claims on the TRICARE-Overseas.com provider portal, you must be enrolled in TRICARE-Overseas.com
If you are already enrolled, click here to initiate submitting claims in TRICARE-Overseas.com.
WPS Health Insurance and WPS Health Plan portal
Qualified providers can view status of claims and customer eligibility.
To register for access to view claim status and/or customer eligibility for the WPS Health Insurance or WPS Health Plan portals, click here.